Degenerative = relating to deterioration over time*
Disc = one of the disk-shaped cushions between the bones of the spinal cord
Disease = a specific problem with a body or body part
* (Note that the word “degenerative” in “degenerative disc disease” doesn’t mean that the pain will keep getting worse over time. That is, the “disease” itself is not degenerative. Instead, “degenerative” describes the cause of the changes in the spinal discs. The changes in the spinal discs are due to wear and tear over time—not to trauma, infection, or some other cause.)
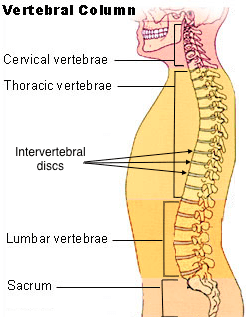 The vertebral column (backbone) is made up of 33 vertebrae. These vertebrae are grouped into divisions called the cervical (neck), thoracic (upper back), and lumbar (lower back). Each pair of vertebrae are connected by an intervertebral disc–a fibrous disc with a softer cartilage core. In a healthy spine, these intervertebral discs cushion the vertebrae and permit normal flexibility of the spine. The vertebral column (backbone) is made up of 33 vertebrae. These vertebrae are grouped into divisions called the cervical (neck), thoracic (upper back), and lumbar (lower back). Each pair of vertebrae are connected by an intervertebral disc–a fibrous disc with a softer cartilage core. In a healthy spine, these intervertebral discs cushion the vertebrae and permit normal flexibility of the spine.
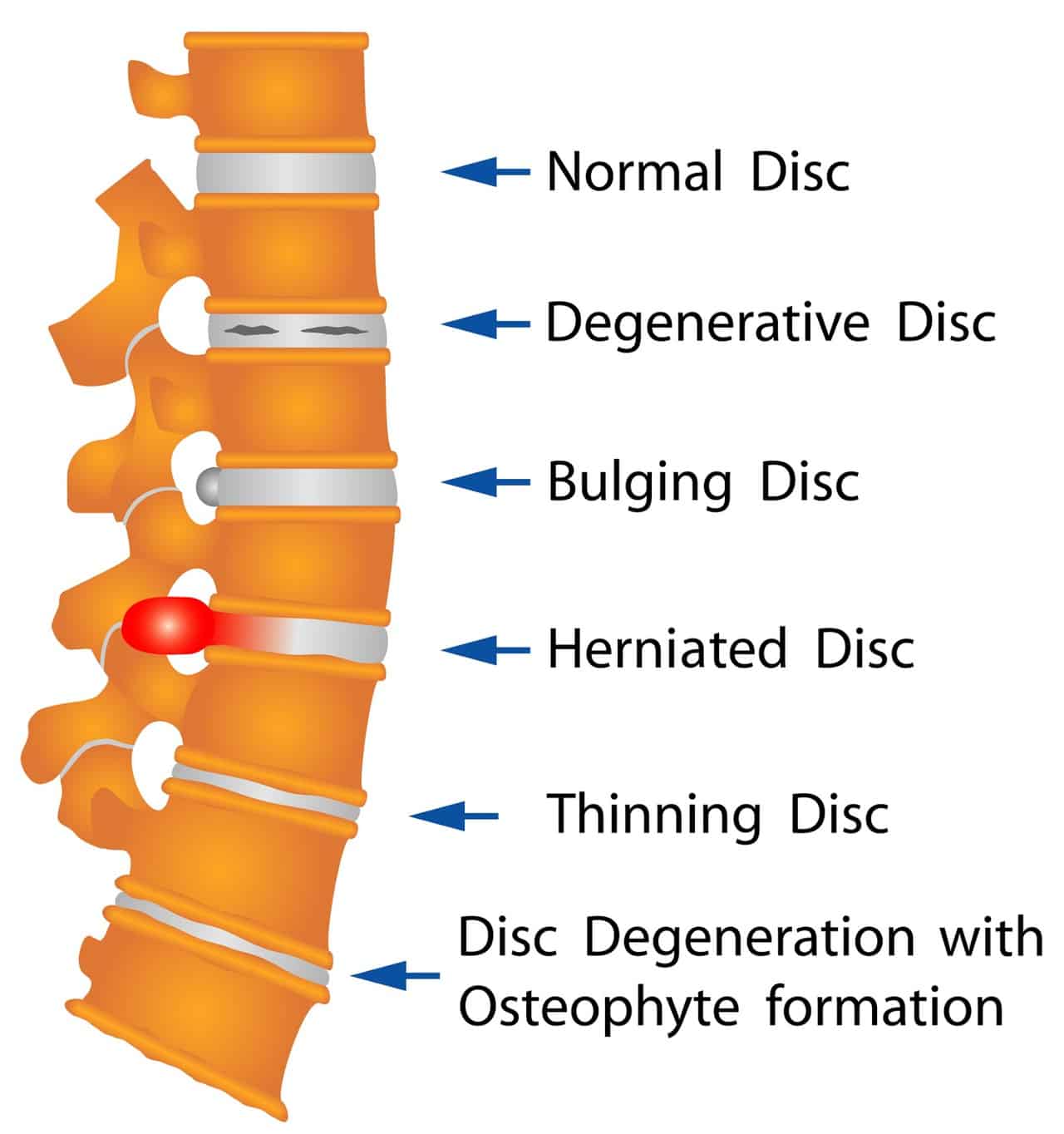
As people age, however, the discs undergo changes. They may dry out, thin, or crack. The soft cartilage core may bulge or herniate out through the fibrous outer portion of the disc. Degenerative disc disease is an umbrella term that describes these age-related processes.
Most people’s spinal discs degenerate over time. By the age of 35, approximately 30% of people will show evidence of disc degeneration at one or more levels. By the age of 60, more than 90% of people will show evidence of some disc degeneration. Degeneration itself is normal, and does not necessarily cause pain. Painless degeneration is just called degeneration. The term “degenerative disc disease” describes disc degeneration that causes pain and other symptoms.
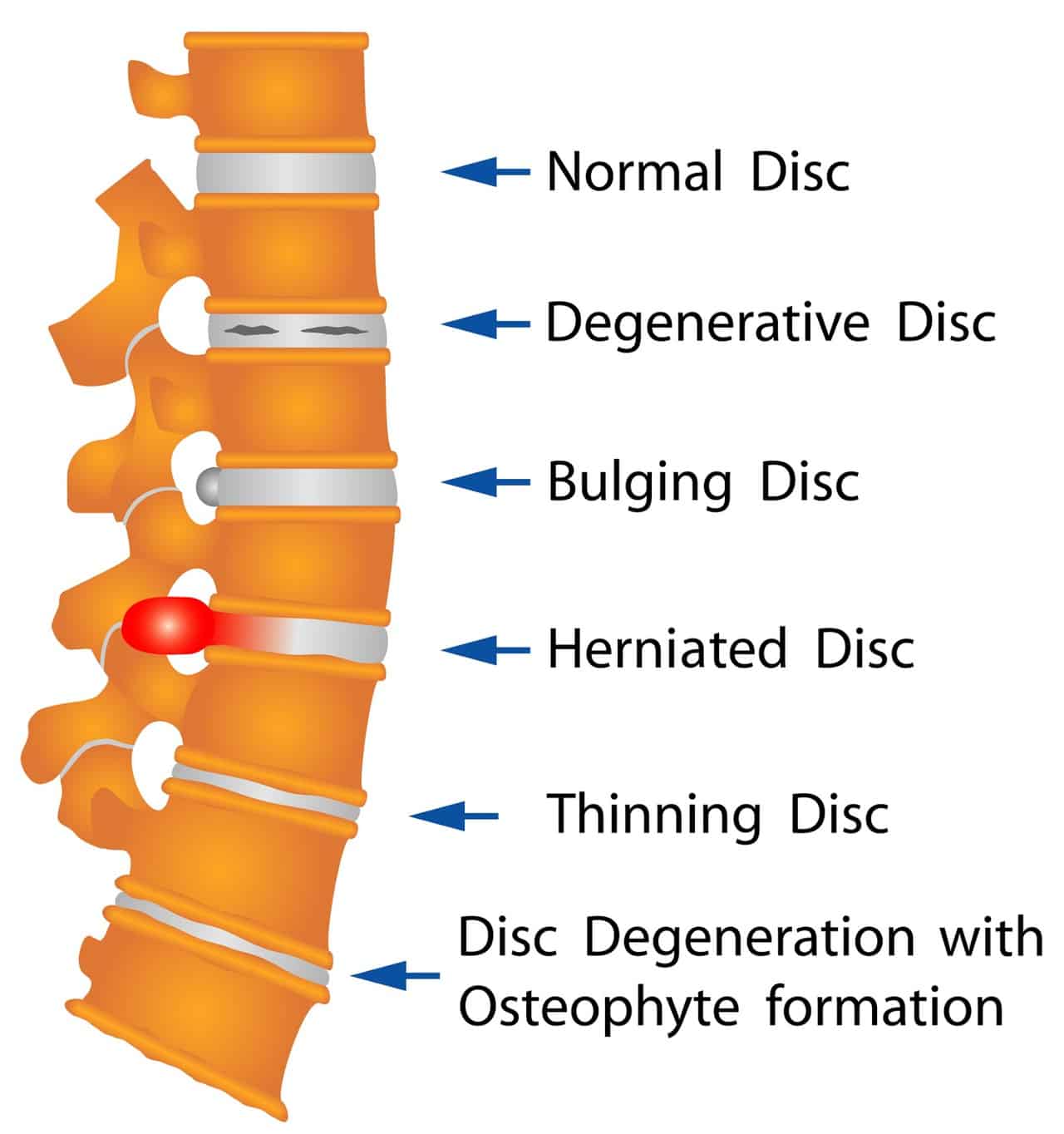 Image courtsey of Anatoly Shevkunov | Dreamstime.com | 
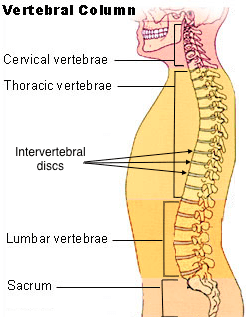 The vertebral column (backbone) is made up of 33 vertebrae. These vertebrae are grouped into divisions called the cervical (neck), thoracic (upper back), and lumbar (lower back). Each pair of vertebrae are connected by an intervertebral disc–a fibrous disc with a softer cartilage core. In a healthy spine, these intervertebral discs cushion the vertebrae and permit normal flexibility of the spine.
The vertebral column (backbone) is made up of 33 vertebrae. These vertebrae are grouped into divisions called the cervical (neck), thoracic (upper back), and lumbar (lower back). Each pair of vertebrae are connected by an intervertebral disc–a fibrous disc with a softer cartilage core. In a healthy spine, these intervertebral discs cushion the vertebrae and permit normal flexibility of the spine.