| Header | Text |
| Overview | This page provides an overview of spinal anatomy, a quick glossary, a description of symptoms that prompt evaluation by a neurosurgeon, and an explanation of common tests and treatments for degenerative spine conditions.
The Spine Hospital at The Neurological Institute of New York is recognized around the world as a leader in the treatment of degenerative spine conditions.
Degenerative spine conditions all involve a loss of normal structure and function in the spine. Degenerative means that the cause of these changes is age-related wear and tear. The changes are not due to trauma, infection, or some other cause.
|
| Spinal Anatomy | To understand degenerative spine conditions, it helps to understand a little about basic spinal anatomy.
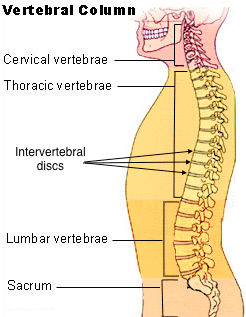
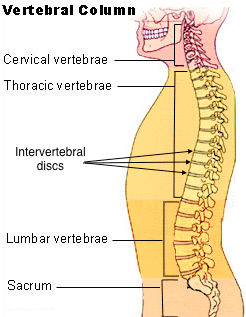 The spine is composed of many vertebrae, or individual bones of the spine, stacked one on top of another. Together, this stack forms the vertebral column. The topmost section of the vertebral column, the section in the neck, is called the cervical spine. The next section, located in the upper and mid-back, is called the thoracic spine. (The vertebrae of the thoracic spine articulate with, or form joints with, the ribs.) Below the thoracic spine is the lumbar spine, in the lower back. Finally, the sacral spine is located below the small of the back, between the hips. Sturdy intervertebral discs connect the vertebrae. The intervertebral discs act as cushions and shock absorbers between the vertebrae. Each disc is composed of a jelly-like core surrounded by a fibrous outer ring. The spine is composed of many vertebrae, or individual bones of the spine, stacked one on top of another. Together, this stack forms the vertebral column. The topmost section of the vertebral column, the section in the neck, is called the cervical spine. The next section, located in the upper and mid-back, is called the thoracic spine. (The vertebrae of the thoracic spine articulate with, or form joints with, the ribs.) Below the thoracic spine is the lumbar spine, in the lower back. Finally, the sacral spine is located below the small of the back, between the hips. Sturdy intervertebral discs connect the vertebrae. The intervertebral discs act as cushions and shock absorbers between the vertebrae. Each disc is composed of a jelly-like core surrounded by a fibrous outer ring.
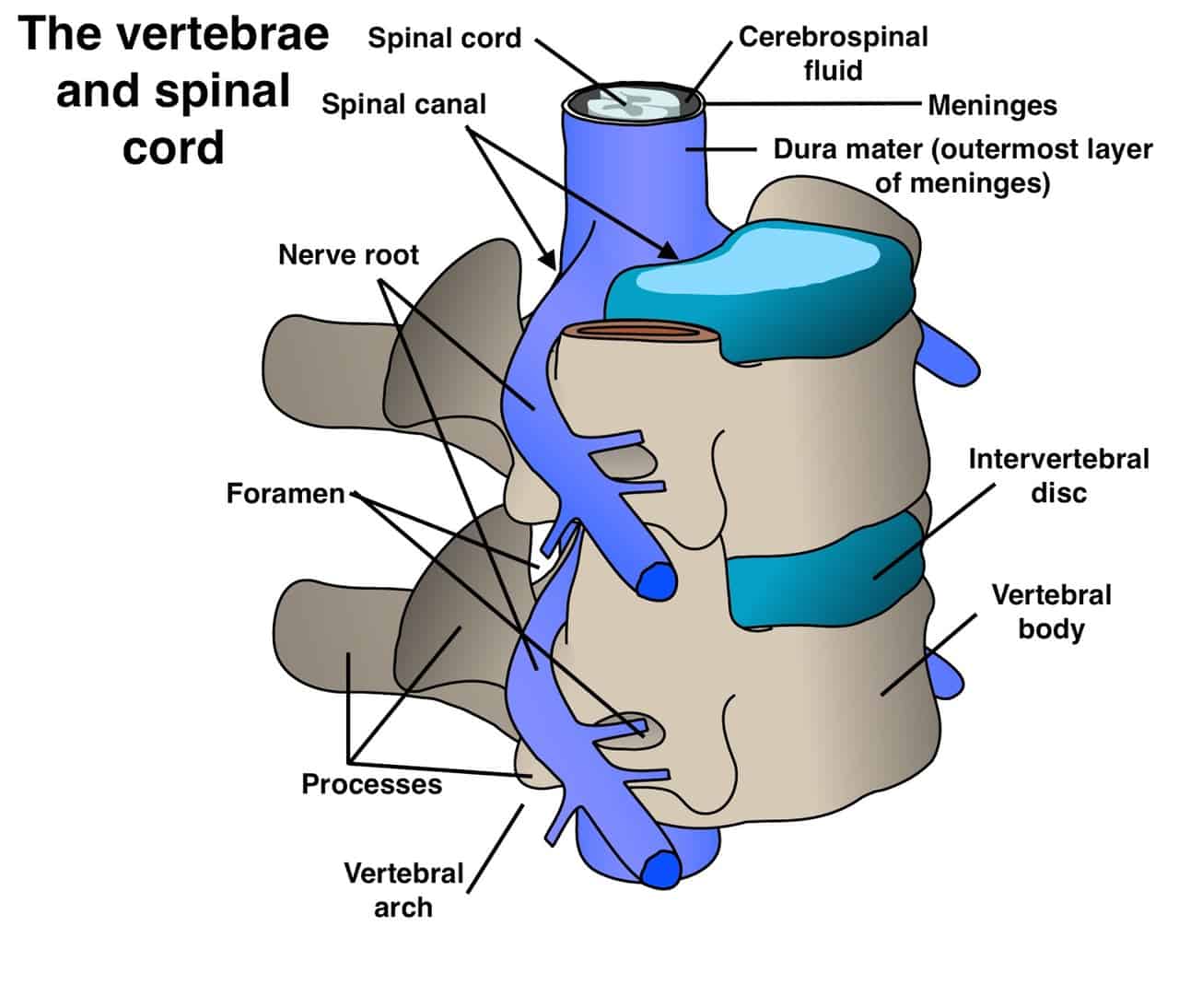
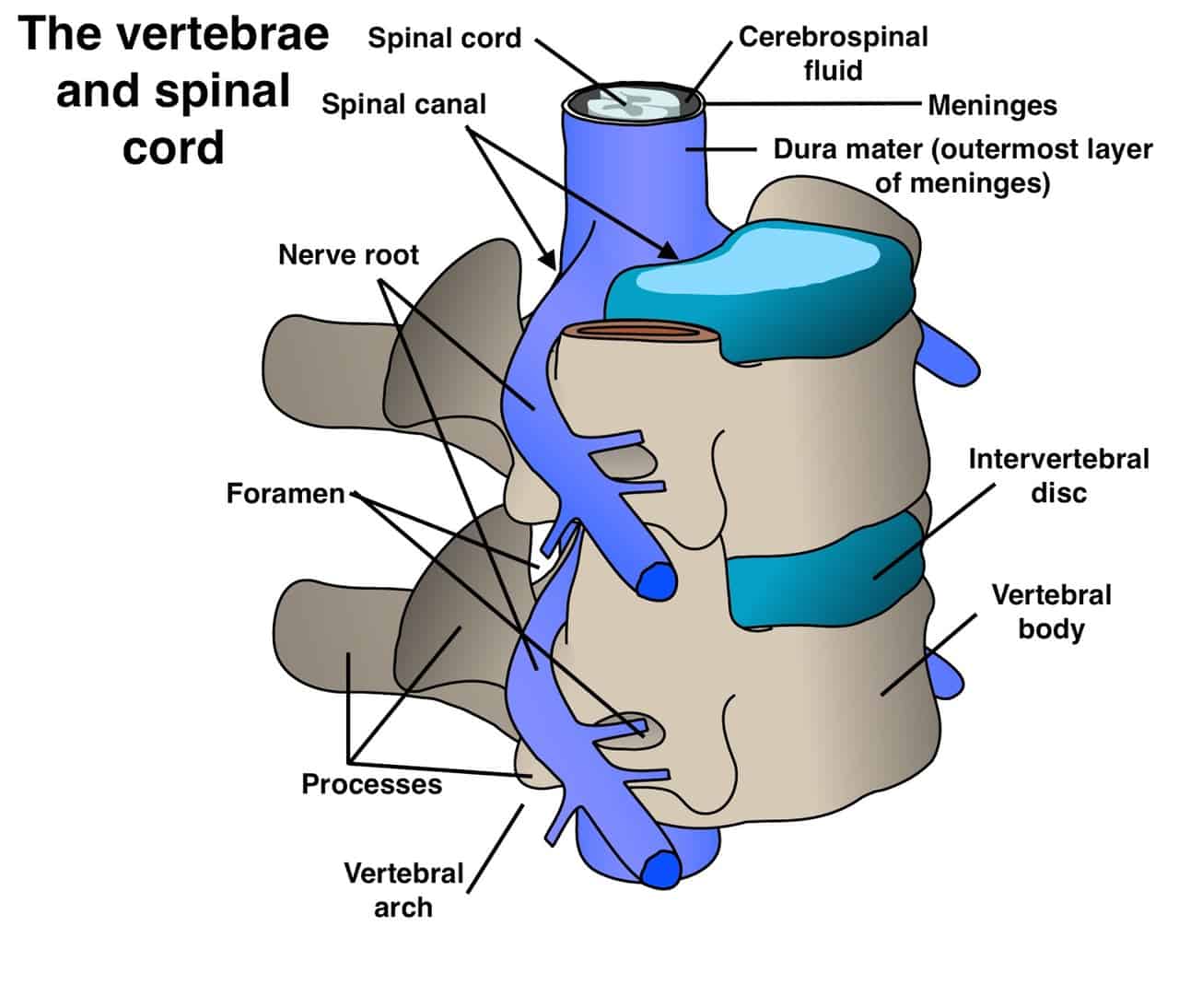
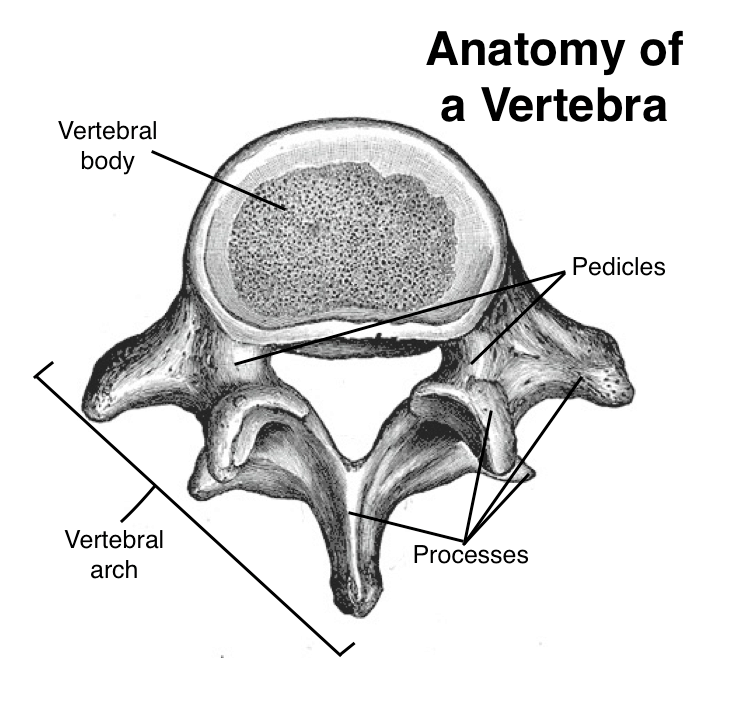 In the cervical, thoracic, and lumbar spine, all vertebrae are essentially similar. Each vertebra (the singular of vertebrae) is composed of two sections. One, the vertebral body, is a solid, cylindrical segment, shaped something like a marshmallow. It provides strength and stability to the spine. The other segment is an arch-shaped section of bone called the vertebral arch. Projecting from the back of the vertebral arch are segments of bones, called processes, that articulate with each other and provide attachment points for muscles, ligaments and tendons. The vertebral arch is connected to the vertebral body by two small columns of bone called the pedicles. Together, the vertebral body, the pedicles, and the vertebral arch form a ring of bone around a hollow center. Stacked on top of one another in the spinal column, these rings align to form a long, well-protected channel known as the spinal canal. In the cervical, thoracic, and lumbar spine, all vertebrae are essentially similar. Each vertebra (the singular of vertebrae) is composed of two sections. One, the vertebral body, is a solid, cylindrical segment, shaped something like a marshmallow. It provides strength and stability to the spine. The other segment is an arch-shaped section of bone called the vertebral arch. Projecting from the back of the vertebral arch are segments of bones, called processes, that articulate with each other and provide attachment points for muscles, ligaments and tendons. The vertebral arch is connected to the vertebral body by two small columns of bone called the pedicles. Together, the vertebral body, the pedicles, and the vertebral arch form a ring of bone around a hollow center. Stacked on top of one another in the spinal column, these rings align to form a long, well-protected channel known as the spinal canal.
Inside the well-protected spinal canal is the spinal cord, the delicate bundle of nerves and other tissue that connects brain and body. The spinal canal also houses the beginning of the spinal nerve roots. These are the nerves that leave the spine, exiting the spinal canal through foramina (small openings) to branch out to the body. The spinal cord and nerve roots are suspended in a liquid called the cerebrospinal fluid. Membranes called the meninges act somewhat like the casing on a sausage, wrapping up the spinal cord, the nerve roots, and the CSF inside the spinal canal. The outermost layer of the meninges is a tough tissue layer known as the dura mater.
Degenerative spinal changes can affect almost every structure of the spine. For example:
- Discs: Intervertebral discs usually change with age. They lose some of their ability to cushion the joints, and their fibrous outer portions may crack, allowing some of the jelly-like core to protrude. This condition is called a herniated disc. They may also slightly collapse and dry out, a condition called degenerative disc disease.
- Bones and cartilage: As cartilage at the joints wears down, the vertebrae or the bony processes at the back of the vertebral arch may rub against one another. This stimulates the growth of bone spurs (extra bone) that may restrict the joints’ range of motion, may cause stiffness and pain, and may compress the nerve roots and spinal cord.
- Ligaments: Ligaments may thicken, causing stiffness and pain or compressing nerve roots or the spinal cord.
|
| Glossary |
- Compression: To neurosurgeons, compression means harmful pressure on the spinal cord or nerve roots. Bone spurs, thickened ligaments, and herniated discs are all possible sources of compression. (Each of these conditions can also exist without causing compression.)
- Myelopathy: A reduction in the spinal cord’s ability to send signals between brain and body. Causes weakness, numbness, clumsiness, and/or bowel and bladder incontinence. Can be caused by compression of the spinal cord.
- Radiculopathy: A reduction in a nerve root’s ability to send signals between spinal cord and body. Causes pain, weakness, or numbness in the area served by that nerve root–for example, the arms or the backs of the legs. Can be caused by compression of a nerve root.
- Stenosis: a narrowing of the spinal canal. Stenosis can compress the spinal cord or nerve roots and may lead to myelopathy or neurogenic claudication.
- Arthritis: joint inflammation that causes pain and stiffness. The most common type is osteoarthritis, which occurs when cartilage in the joints wears down.
- Bone spurs: extra bone that may grow on joints affected by osteoarthritis. Bone spurs may compress the spinal cord or nerve roots.
- Nonsurgical treatments: Treatments such as physical therapy, medication, heat and cold, etc. Nonsurgical treatments avoid the risks of surgery, and are the best choice for certain cases of degenerative conditions. Arthritis and disc herniation, for example, are best treated nonsurgically when they do not cause spinal cord or nerve root compression. (Also called nonoperative treatments.)
- Surgical treatments: Surgical treatment is necessary to treat compression that causes myelopathy and certain cases of radiculopathy. While there are many specific procedures that remove pressure from the spinal cord and nerve roots, they may be grouped under the general heading of decompressive surgery.
|
| Symptoms | Degenerative spine conditions vary widely in their presentation. Some cause no symptoms at all. When symptoms do occur, they often include back pain or neck pain. Other symptoms depend on the location and type of problem.
Many degenerative conditions do not require surgical treatment, but some may. “Red flags” for evaluation by a neurosurgeon include:
- Back pain accompanied by bowel or bladder incontinence and/or numbness in the areas that would sit on a saddle (so-called saddle anesthesia)—may indicate cauda equina syndrome, a rare neurological condition that should be treated promptly
- Neck or back pain that includes weakness, numbness, or pins-and-needles in the arms or legs–may indicate myelopathy
- Neck or back pain that radiates (spreads) into the shoulder, arm, hand, leg, or foot–may indicate radiculopathy
- Neck or back pain accompanied by fever
- Neck or back pain that gets worse during the night
- Neck or back pain accompanied by unexplained weight loss
- Neck or back pain that continues for several weeks or months
- Neck pain accompanied by difficulty breathing or swallowing
- Neck or back pain following a fall, injury or other trauma
|
| Tests and Diagnosis | If a patient presents with symptoms associated with degenerative spine disorders, the doctor may order the following tests:
- X-ray (also known as plain films) –test that uses invisible electromagnetic energy beams (X-rays) to produce images of bones. Soft tissue structures such as the spinal cord, spinal nerves, the disc and ligaments are usually not seen on X-rays, nor are most tumors, vascular malformations, or cysts. X-rays provide an overall assessment of the bone anatomy as well as the curvature and alignment of the vertebral column. Spinal dislocation or slippage (also known as spondylolisthesis), kyphosis, scoliosis, as well as local and overall spine balance can be assessed with X-rays. Specific bony abnormalities such as bone spurs, disc space narrowing, vertebral body fracture, collapse or erosion can also be identified on plain film X-rays. Dynamic, or flexion/extension X-rays (X-rays that show the spine in motion) may be obtained to see if there is any abnormal or excessive movement or instability in the spine at the affected levels.
- Magnetic resonance (MR) imaging – provides a detailed image of soft tissue like discs, nerves and the spinal cord. This scan allows the doctor to see how the nerves and spinal canal space are affected by degenerative spine conditions.
- Computed tomography (CT) scan – provides a detailed image of bone structures in the spine. A CT scan uses computers and X-rays, and provides much more detail than a plain X-ray.
- Myelography / post myelogram CT – provides images that can help determine whether bulging or herniated discs are compressing the spinal cord or nerve roots. Performed by injecting a contrast dye into the spinal column and taking several X-rays and, usually, a CT scan.
- Electromyography (EMG) – tests the electrical activity of a nerve root to help determine the cause of pain.
- Discogram – helps determine whether pain is due to a damaged intervertebral disc. Performed by injecting a contrast dye into the disc and taking several X-rays while also asking the patient about symptoms.
|
| Treatments | Since the causes of degenerative spine conditions will vary from patient to patient, no two treatments will be identical.
Before surgery is considered, nonoperative treatments may be recommended. These measures include:
- Medications (pain medications, anti-inflammatory medications, antidepressants, anticonvulsants, non-steroidal anti-inflammatory drugs (NSAIDs), topical opioids, and/or epidural injections of steroids or pain medication)
- Bracing
- Activity modification
- Patient education on proper body mechanics (to help decrease the chance of worsening pain or damage to the disc)
- Physical therapy (will focus on strengthening the muscles of the back/neck and improving flexibility as well as range of motion)
- Weight control
In some cases, surgery may be recommended or required to treat a degenerative condition. The type of procedure depends on the type of condition and its severity. Surgery is considered when:
- A patient’s symptoms do not respond to nonoperative measures
- A patient’s pain is severe
- Myelopathy is present
In such cases, surgery has the potential to relieve pain, prevent further damage to the spinal cord, and drastically improve a patient’s quality of life. Procedures include:
In some situations, the surgeon may also need to perform a spinal fusion to ensure the spinal column is stable. During a spinal fusion, the surgeon will place a bone graft between the vertebrae to cause the bones to fuse (grow together).
For a detailed explanation of specific degenerative spine conditions, refer to the individual pages.
|
| Preparing For Your Appointment | Drs. Paul C. McCormick, Peter D. Angevine and Dr. Patrick C. Reid are experts in treating degenerative spine conditions. They can also offer you a second opinion.
|

 The spine is composed of many
The spine is composed of many 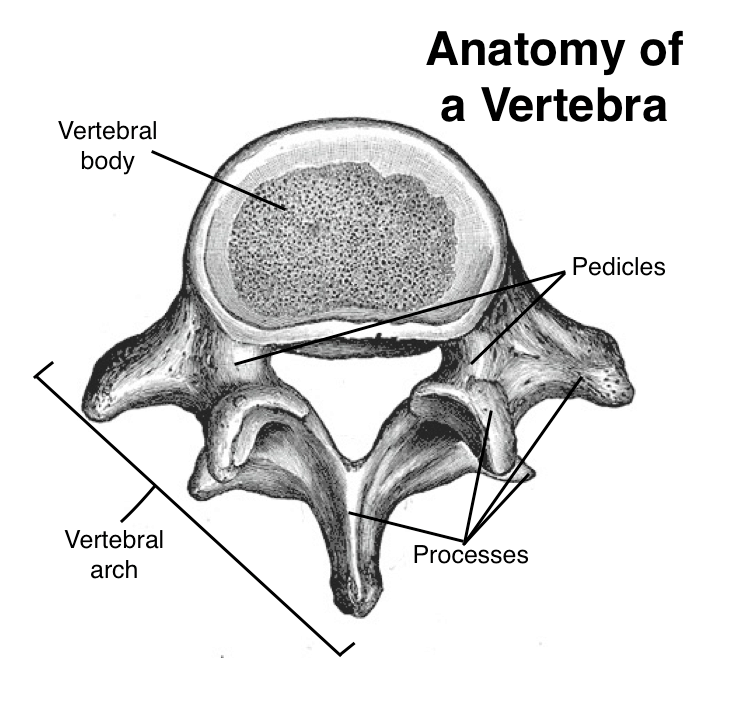 In the cervical, thoracic, and lumbar spine, all vertebrae are essentially similar. Each
In the cervical, thoracic, and lumbar spine, all vertebrae are essentially similar. Each